
About
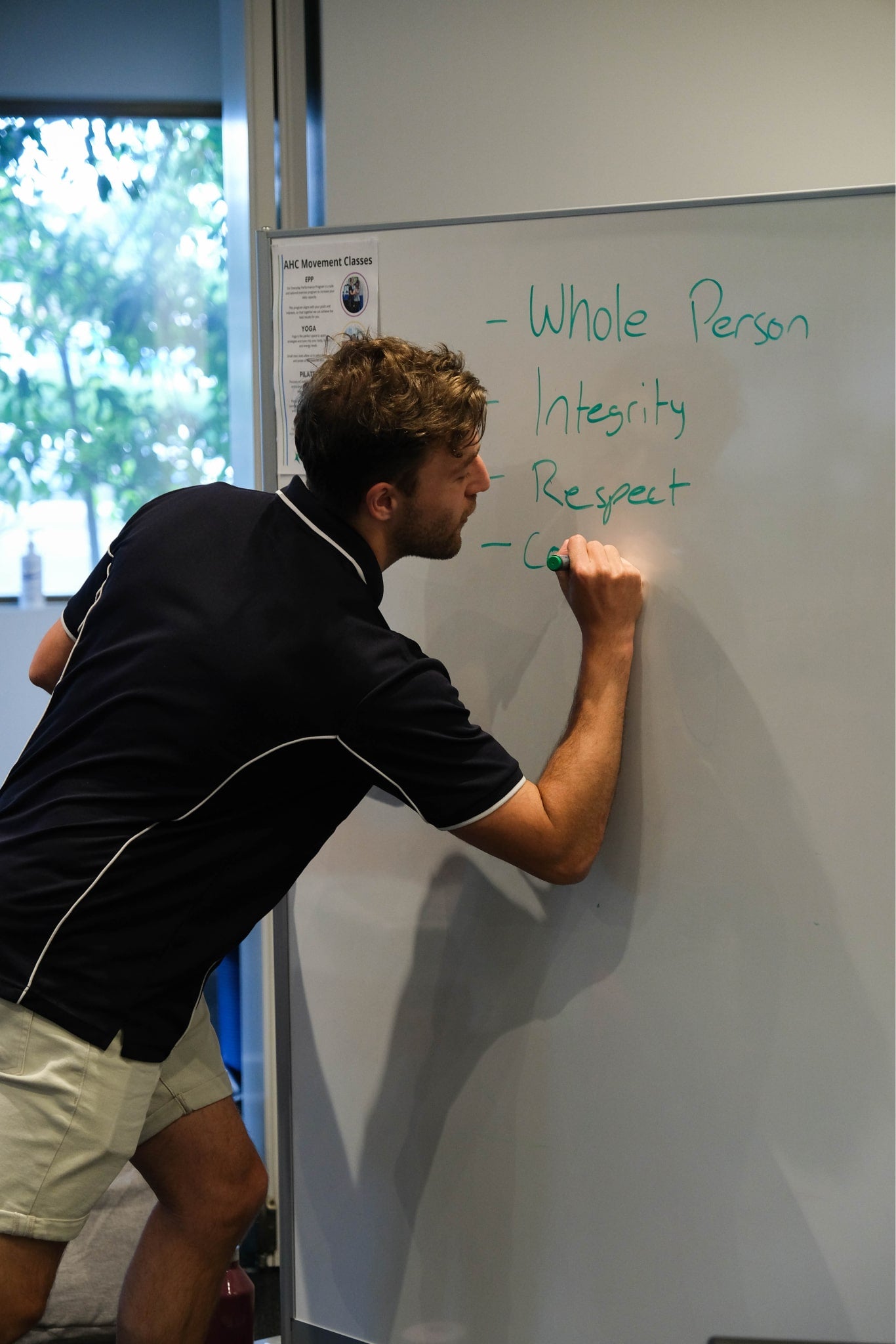
Pain can invade our everyday lives and limit the things we love to do. Here at Active Health Clinic, we pride ourselves on the rehabilitation and management of fibromyalgia, chronic pain and a range of other conditions that are seen as ‘too hard’ or don’t fall into a traditional category or treatment approach.
Our tailored and individual programs are designed for you to manage your condition and progress towards your goals. We teach you guidelines, not rules, which you can follow for the rest of your life. Unfortunately there are no 'quick fixes' for fibromyalgia or chronic pain, however, research shows that a combination of the programs we offer have can provide significant improvements in your symptoms and function.

Program background
Fibromyalgia and Chronic Pain
Our Program
Cost and questions
Dietetics in Chronic Pain and Fibromyalgia

What Our Patients Are Saying
Ready to get started?
Wishlist
Wishlist is empty.
Wishlist
Compare
Shopping cart
Your cart is empty.
Return to shop


