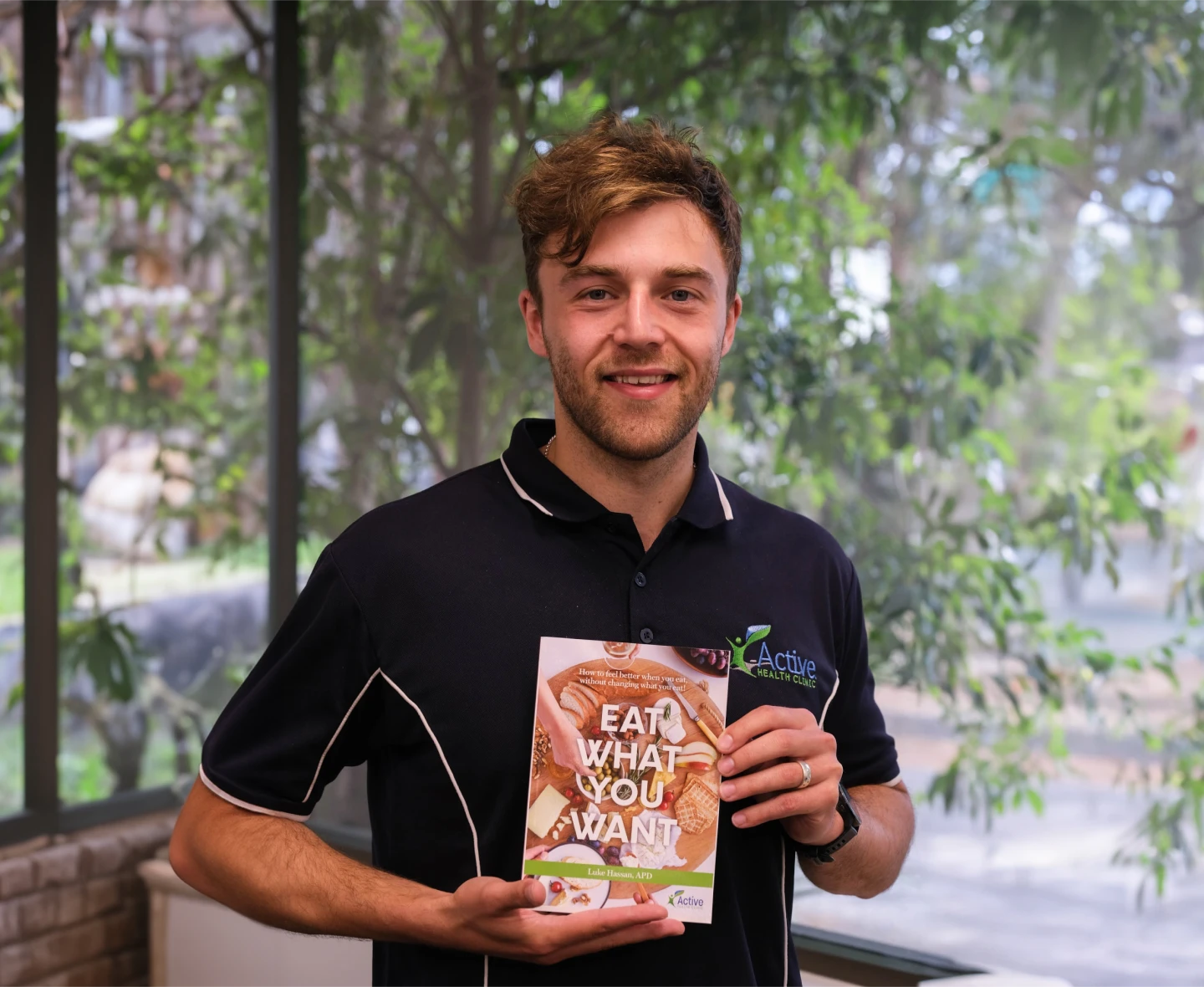
The AHC Sleep Program

Real Talk From Our Sleep Experts
What is the Program?

Your Program, Tailored to You
Title
The Food - Sleep Connection


What Are Sleep Disorders?
Sleep disorders are conditions that disrupt your natural sleep patterns, making it difficult to fall asleep, stay asleep, or feel rested during the day, for some this can also be an increase in sleep needs. They can affect your energy, mood, and overall well-being.



Common types of Sleep Disorders


Sleep-Related Breathing Disorders
How They Affect You

Central Disorders of Hypersomnolence
How They Affect You

What causes poor sleep?

Poor sleep depth
Irregular sleeping times
Not getting enough sleep
A sleep disorder
Are You Missing a Diagnosis?
Our programs are tailored to YOUR symptoms
Wishlist
Wishlist is empty.
Wishlist
Compare
Shopping cart
Your cart is empty.
Return to shop