About
Dysautonomia, including Orthostatic Intolerance (OI) and Postural Orthostatic Tachycardia Syndrome (POTS), involves dysfunction of the autonomic nervous system, which regulates essential bodily functions like heart rate, blood pressure, and digestion.
POTS is characterised by an increased heart rate upon standing, leading to symptoms like lightheadedness, fainting, and exercise intolerance. OI refers to difficulty tolerating an upright posture, often resulting in dizziness and low blood pressure.
These conditions can significantly impact daily life, but understanding and managing them through symptom-focused treatment can improve quality of life.
Managing your OI & POTS symptoms

Orthostatic Intolerance & POTS
Symptoms of OI & POTS:
These symptoms can be exacerbated by numerous factors including dehydration, heat exposure, prolonged recumbency, alcohol, and menstruation.
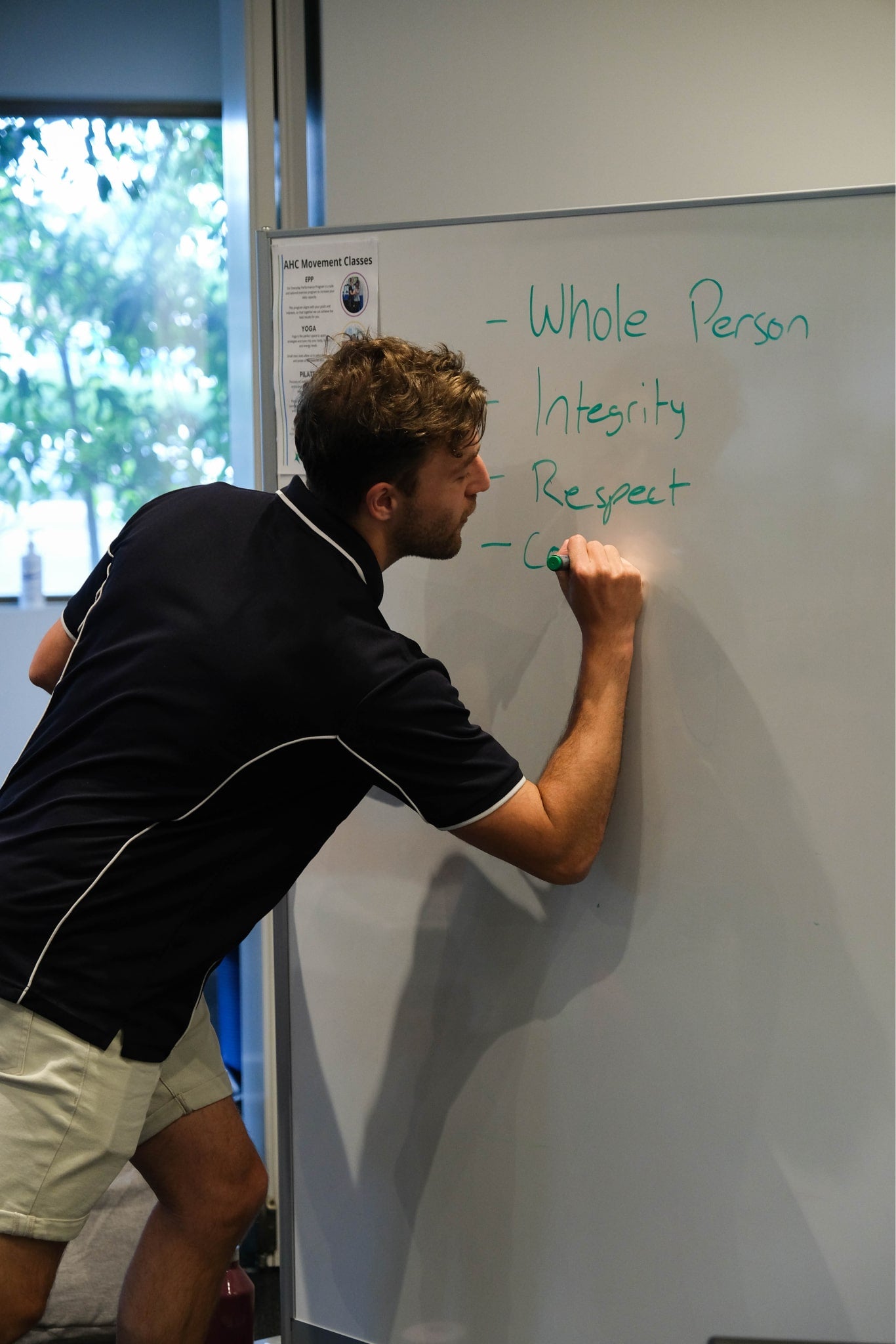
Our Program
Title
Title
Cost and questions
Dietetics in Dysautonomia


Ready to Take Control of Your Health?
What Our Patients Are Saying
Ready to get started?
Wishlist
Wishlist is empty.
Wishlist
Compare
Shopping cart
Your cart is empty.
Return to shop


